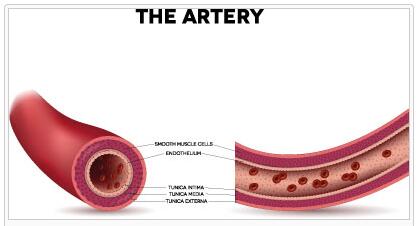
As aortic dissection is a detachment of the inner wall layer of the aorta, the intima, designated by the called Media central wall layer. Most aortic dissection is based on an injury or a tear in the intima, which form the entry point for bleeding. The bleeding can lead to an expansion of the dissection and a rupture of branching arteries with all the ensuing consequences.
What is an aortic dissection?
With an aortic dissection, the inner layer of the vessel wall separates from the middle one.
According to lawfaqs, aortic dissection is a splitting of the three-layered vessel walls of the aorta . The starting point for the development of an aortic dissection is usually a tear or a lesion of the inner wall, the intima. The tear or lesion forms the gateway for bleeding between the intima and adventitia, the outer vessel wall or into the middle layer, the media.
Because of the bleeding between the wall layers associated with the dissection, the aortic dissection is also aptly referred to as aneurysm dissecans aortae or burrowing bleeding . About 60 percent of the immediately life-threatening dissection affects the ascending branch of the aorta. In rarer cases, however, an aortic dissection can occur in any part of the aorta.
The hemorrhage creates a double lumen that can tear off branching arteries. This means that their target areas can no longer be supplied with arterial blood and are threatened by acute oxygen deficiency ( ischemia ).
The bleeding, which pulsates with the heartbeat, allows the aortic dissection to spread further within the aortic walls and cause severe damage. In principle, the dissection can extend over a few millimeters to several centimeters or, in extreme cases, over the entire length of the aorta.
Causes
The most common cause of the development of an aortic dissection is seen as an arteriosclerotic change in the intima or in a degenerative weakness of the media. The elasticity of the intima is reduced by arteriosclerotic changes. This leads to constrictions of the aorta in the course of its air kettle function.
In extreme cases, the vasodilatation, which is constantly taking place in the rhythm of the heartbeat, can suffer a tear. Another possible complex of causes is media degeneration , which can arise from untreated chronic high blood pressure or, in rarer cases, from congenital weakness of the connective tissue of the media.
The genetically determined media degeneration leads to a loss of its elasticity, so that the aorta no longer narrows properly after the passive vasodilation during ventricular systole. The media looks like it is “worn out”, so that the intima is exposed to strong stretching loads, which can cause a tear and subsequent bleeding.
Symptoms, ailments & signs
Symptoms and complaints of aortic dissection cover a wide range from unnoticeable to sudden death. Sudden death can result from a rupture of the ascending aorta or from occlusion of a coronary artery. In the vast majority of cases of aortic dissection, sudden onset of severe pain occurs.
These are usually described as tearing or stabbing and are perceived as extremely threatening by those affected. The localization of the pain provides initial clues as to the section of the aorta affected by the dissection. Often the acute pain is so severe that it leads to unconsciousness .
Further symptoms such as shortness of breath , pain in the extremities, signs of a stroke and symptoms of paralysis can occur in addition to the main symptoms.
Diagnosis & course
If there is an initial suspicion based on the leading symptoms, x-ray and ultrasound examinations , especially transesophageal echocardiography (TEE), can provide further information. Computed tomography (CT) and magnetic resonance tomography (MRT) provide even more detailed images . The course of an aortic dissection is unpredictable.
In some cases, the blood between the walls finds its way back into the “correct” lumen through a further opening in the intima, so that the acute risk of an expansion of the dissection is reduced. In other cases, the dissection progresses in bursts, so that other supply areas such as the extremities, kidneys and digestive organs are affected.
There are also cases known in which a thrombus closes the opening in the intima and thus leads to an apparent self-healing. The most dangerous course occurs when the outer layer of the wall, the adventitia, is widened so much by the bulge between the walls that it tears and almost all of the blood in the body’s circulatory system can escape from the aorta and lead to fatal bleeding to death within a very short time.
Complications
Untreated aortic dissection can cause a number of serious complications, including sudden death. The type of aortic dissection is critical to the type of complications that arise as a result. The slightest complications arise when the bleeding into the space between the inner wall (intima) and the media, the elastic middle wall of the aorta, finds its way back into the “correct” lumen of the aorta after only a short distance.
In this case, the cascade of mutually reinforcing symptoms and complications is initially interrupted. It is possible that a very small aortic dissection may in exceptional cases remain without symptoms or complications. In the vast majority of cases, aortic dissection is accompanied by sharp pain, which can be so severe that a temporary loss of consciousness occurs.
The development of further complications depends on the course of the dissection. In those cases in which it causes a severe stenosis, the further complications result from insufficient blood flow to the internal organs such as the liver, kidneys and intestines as well as the lower part of the body. Particularly serious and immediately life-threatening complications can arise if the aortic dissection takes a progressive course.
The entire length of the aorta may be affected by the bleeding. There is then also the increased risk of a rupture of the aorta with the risk of internal bleeding resulting in death.
When should you go to the doctor?
The symptoms of an aortic dissection range from barely noticeable to sudden death, because the extent of the bleeding between the inner wall of the aorta (intima) and the middle wall (media) can be very different. A diagnosed aortic dissection requires immediate action because the progression and thus further complications cannot be predicted. The progression of the disease depends primarily on the factors causing the aortic dissection.
There is always the danger that the splitting off of the intima from the media will expand in a matter of minutes due to the pulsating blood pressure between systole and diastole and lead to an immediately life-threatening situation. A slight relaxation is only called for when the blood that penetrates between the intima and media can flow back into the “correct” lumen of the aorta through a second crack in the intima. The risk of an unpredictable expansion of the aortic dissection is significantly reduced by the backflow of blood.
Postponing any necessary further diagnostic examinations using imaging procedures such as MRI can be life-threatening because in some situations only a quick, surgical procedure can save life. There is not a single clinical picture conceivable that could justify postponing treatment in an appropriately equipped clinic. The clinic should have the necessary diagnostic procedures and invasive or minimally invasive treatment options.
Treatment & Therapy
After diagnosing an acute aortic dissection, the most important measure is to prevent an impending rupture of the aorta. This means that first antihypertensive measures should reduce the systolic pressure to 110 mmHg. At the same time, pain reliever drugs are used.
If the dissection is located in the ascending branch of the aorta, surgical replacement in this area with an artificially manufactured vascular prosthesis is usually urgently indicated. If the dissection is limited to the descending branch of the aorta and is therefore less threatening, treatment consists initially of drug therapy. With a more detailed analysis and localization of the dissection, so-called percutaneous intimal membrane fenestration (PFA) can also be used.
Stents are inserted via percutaneously inserted catheters and the intimal tears are practically glued to the stents. An attempt is often made to dilate, reposition and restore function of blocked or sheared arterial branches during the procedure.
Outlook & forecast
The prognosis for an aortic dissection carries a high risk of death in all forms, although this has improved significantly in recent decades. While the disease was almost always fatal almost 50 years ago, today less than 20% of people die from the defect within a month of the occurrence. Without medical care and surgery, around half of those affected have a fatal outcome.
The likelihood of survival from an aortic dissection increases if immediate medical care is initiated in the event of an acute health condition. It is also helpful to have blood pressure and general condition checked at regular intervals and precautionary measures taken. This reduces mortality.
With increasing age, the risk of an aortic defect increases significantly due to age. Most of the people affected are on average over 65 years of age. With a vascular prosthesis and drug treatment, the sick have a comparatively good prognosis. Nevertheless, within the first year after the dissection, around 10% of patients still die.
In addition, patients must expect life-limiting measures. You are physically and emotionally less resilient. Excitement, stress and hecticness increase the risk and there is an increased risk of further vascular damage and renewed aortic dissection.
Prevention
There are few preventive measures that cannot completely eliminate the risk of aortic dissection, but at least reduce it. It is particularly important to keep the systolic blood pressure at a normal value of 120 to 140 mmHg and to use ultrasound to examine the carotid arteries (arteria carotis) for possible deposits (plaques) at regular intervals of one to two years (depending on age).
This is especially true if there is a genetic defect that leads to degeneration of the middle layer of the vessels, the media, and increases the risk of aortic dissection in the long term.
Aftercare
Regular follow-up care is extremely important for patients with aortic dissection. Intervals between three and six months are recommended, after which a follow-up examination should be carried out annually. During this examination, the blood pressure is checked or, if necessary, adjusted to values around 120/80 mmHG.
A contrast CT scan is also performed to check the aorta and document the course of the disease. It is very important to have an overall view of the aorta in order to be aware of any changes in diameter or newly added hematomas. If necessary, an enlarged main artery can be discovered at an early stage and treatment can be carried out quickly.
About a third of people will either progress or develop an aortic rupture (tear in the aortic wall) within five years and require further surgical treatment. Sufferers with implanted coronaries (coronary arteries) have to undergo regular ergometric follow-ups.
If there is a suspicion of stenosis (narrowing of a blood vessel), a coronary angiography (radiological vascular imaging) must be performed. Echocardiography should be performed annually in patients whose heart valves have been reconstructed. In addition, regular organ controls, neurological controls and pulse status controls are recommended.
You can do that yourself
There are several things to consider for patients after aortic dissection. The procedure not only affects the cardiac output and the associated condition, but also the surrounding chest muscles. It is therefore appropriate to strengthen them. It is important, however, that this is done gently in the beginning.
For this, a Theraband can be used, which is wrapped around the wrists and strengthens the upper arm muscles and thus indirectly the chest muscles through slight external rotation of the wrists. Forced muscle training of the direct chest muscles is only appropriate after about six to eight months.
Boxing and punching movements must be avoided in any case in the first time, as these may cause the transmission of stimuli that can jump from the chest muscles to the heart muscle, which can overstrain the heart. Heavy lifting and pressure breathing should also be avoided, as these too put unnecessary strain on the heart. If possible, coughing should also be converted into coughs to relieve pressure in the chest area.
Individual compliance with these restrictions should always be discussed with the attending physician and physiotherapist . Later you can start with modified push-ups on the wall and light water aerobics to improve your general condition and thus your stamina.